
FH Europe Foundation proud to support Apheresis Awareness Day 2023!
We want to raise awareness about the benefits of apheresis therapy in managing conditions like homozygous familial hypercholesterolemia (HoFH) and high Lp(a) as well as the rare condition familial chylomicronemia syndrome (FCS). We want to highlight the crucial role of apheresis in reducing the risk of cardiovascular events in patients with inherited lipid conditions as well as reducing the risk of acute pancreatitis during pregnancy in patients with FCS. This campaign will grow and we encourage you to share some of your stories. [1]
Learn more about Apheresis and watch the stories from our patients, who are involved in this treatment.
Apheresis treatments for inherited lipid conditions are therapeutic procedures that aim to lower the levels of lipids, such as cholesterol or triglycerides, in the blood. During the procedure, blood is collected from a patient and passed through a machine that separates the plasma from other blood components. In HoFH and Lp(a) the machine then removes the excess lipids from the plasma and returns the remaining blood components to the patient, while in FCS the patient has given donated plasma. This process can be done on a weekly or bi-weekly basis, and each treatment session typically lasts a few hours.

Proteins carry cholesterol throughout the body, forming a combination called lipoprotein. There are two main types of lipoproteins: LDL (low-density lipoprotein), which is harmful and previously referred to as “bad’ cholesterol, and HDL (high-density lipoprotein), which is protective and previously referred to as "good" cholesterol. If you have too much harmful cholesterol in your blood, your risk of getting cardiovascular (heart) disease increases. Another lipoprotein, Lp(a), can also increase the risk of cardiovascular disease if it is raised.
Lipoprotein apheresis is a highly effective procedure designed to remove LDL cholesterol from the bloodstream. This intervention is known to cause only a minimal decrease in HDL levels. It is recommended for individuals who have very high LDL cholesterol levels and already attempted medication therapy and a low-cholesterol diet, but levels of LDL cholesterol remain high.
Moreover, it is the preferred approach for managing elevated Lp(a) levels.
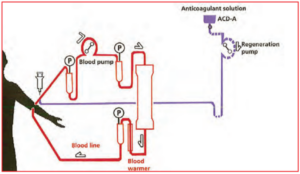
The diagram shows how lipoprotein apheresis is performed.
Apheresis treatments have been shown to effectively reduce lipid levels in patients with inherited lipid disorders, helping to prevent complications such as cardiovascular disease. It is also a treatment used to support patients living with the rare condition FCS during pregnancy.
Lipoprotein apheresis could be an option for you, if:
Lipoprotein apheresis treatment can be done on a weekly or bi-weekly basis, and each treatment session typically lasts a few hours. Patients are treated on an individual basis at a specialized treatment facility. This will also impact on how regular treatments can happen.
Plasma exchange for patients with familial chylomicronemia syndrome (FCS) during pregnancy involves the removal of plasma components that contribute to high levels of triglycerides. By removing excessive triglycerides, this treatment helps reduce the risk of pancreatitis and other complications associated with FCS during pregnancy. The frequency and duration of these treatments vary depending on the patient's condition and response to therapy. Typically, patients undergo treatment once or twice a week for a few hours each session. These treatments can greatly improve the health and well-being of FCS patients during pregnancy. [2]

Apheresis offers hope to patients with high Lp(a) levels and signs of atherosclerosis. [3]
Listen to Krish, an FCS patient from the UK, talking about her experience having lipoprotein apheresis during her pregnancy.
Lipoprotein apheresis can be used for treating children. It means it’s possible to stop high cholesterol from causing damage at an early age. This is important for people with FH with two faulty genes (Homozygous FH, Compound HeFH), which can cause heart disease early in life if it isn’t treated.[4]

Patient Ambassador Avery (age 15) started with apheresis treatments at age 7.
Access to this specialized treatment is very different, depending on the location. It varies not only among countries but also inside every country.
In many areas, the availability of Lipoprotein Apheresis is very limited, largely attributable to the procedure's high cost and the specialized apparatus required. In addition, there is a lack of trained medical professionals who are able to perform this complex procedure, further restricting access for those in need. This also places a higher burden on patients both socially, financially and emotionally.
Inaccessibility to lipoprotein apheresis for example has dire consequences for patients in Lebanon with conditions like Homozygous FH, Lp(a), and FCS during pregnancy. [5]
Listen to Chyrel, our Patient Ambassador living with HoFH talking about problems with limited access to Apheresis treatment in Lebanon.
Lipoprotein apheresis is a procedure that's similar to kidney dialysis. During the procedure, two needles (called cannulae) are inserted into your veins. One needle is used to lead the blood flow from the body and the other is used to return the treated blood back into your body. A portion of your blood is circulating outside of your body using a machine. This machine removes LDL cholesterol and Lp(a) from your blood, and then returns the treated blood back into your body. The machine parts that come in contact with your blood are sterile and are only used once.

In the beginning, your LDL cholesterol and/or your Lp(a) levels will be measured before and after each apheresis treatment. Your blood results will also regularly be reviewed and your treatment will be adjusted as needed to ensure it's working as optimal as possible.
With just one session, lipoprotein apheresis can lower your LDL cholesterol and Lp(a) levels by 50 and up to 70 percent, depending on your initial levels and the amount of blood treated. However, it doesn't address the root cause of high LDL cholesterol and/or high Lp(a). Your levels will start to rise again soon after treatment. To maintain lower levels of LDL/Lp(a), you'll need treatment every two weeks or, in some cases, weekly. Lipoprotein apheresis seems to be a lifelong therapy, so it's important to continue following a low-fat diet and taking all cholesterol medications.
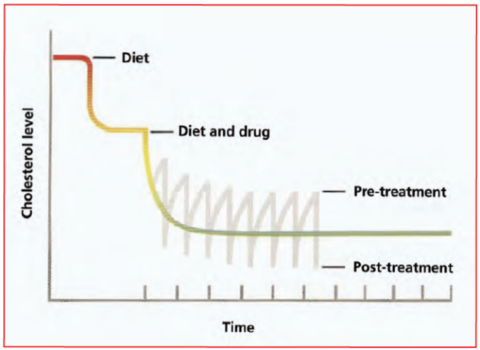
The diagram - combination of diet, medication, apheresis treatment lower cholesterol.
If you have issues with blood flow from your arm veins, you may be offered:
If you need either of these, your doctor will discuss both options with you in more detail.
Heparin or another anticoagulant solution, called ACD-A, can be used to thin your blood before it circulates through the machine.
The blood-thinning medication prescribed will be determined by the type of machine that is used. A temporary decrease in your blood calcium levels may be caused by ACD-A. To prevent this, calcium tablets will be provided to you during each treatment session.
A small number of patients may experience one or more of the following temporary side effects:
The nurses in the unit will be able to help treat any problems or side effects.
For patients with HoFH and Lp(a) you will be advised not to take any beta blocking tablets, including atenolol, propanolol, metoprolol, and bisoprolol, or any other medication to lower your blood pressure before your treatment. You should continue taking your medication as usual the day after your treatment. If you develop anaemia, you may need to take an iron supplement.
If your doctor suggests starting ACE inhibitor medication, such as ramipril, lisinopril, and perindopril, please discuss the effects with him or consult your lipid specialist, as they may interfere with some of the machines used for lipoprotein apheresis. If you are already taking ACE inhibitor medication before starting apheresis, your doctor may need to switch you to an alternative medicine that does not interfere with the machine before starting treatment.
It is important to eat and drink something before your treatment, and you may continue to eat and drink during the procedure. However, please avoid alcohol 24 hours before your treatment, as well as any strenuous exercise on the day of your treatment, and activities that may increase the risk of physical injury for 24 hours after your treatment due to the blood-thinning medication used.
For the first two or three occasions, we recommend that you do not drive to and from your treatment. To further reduce the risk of side effects, it is advisable to rest for the remainder of the day after your treatment.