On 18 April, we mark European Patients’ Rights Day – an important occasion dedicated to raising awareness of patients’ rights and promoting their protection across Europe. Established by Cittadinanzattiva/Active Citizenship Network in cooperation with various European citizens' organisations, the day is grounded in the European Charter of Patients’ Rights, which sets out 14 fundamental rights that should be recognised and respected in all healthcare systems.
This annual day of action reminds us that every person deserves access to safe, respectful and high-quality healthcare. It encourages all those involved in healthcare – from policymakers and professionals to patient advocates and citizens – to work together to protect and advance these rights.
Each year, the day is marked with public events, conferences and initiatives across Europe, often supported by institutions such as the European Parliament and the European Economic and Social Committee. It serves both as a moment to highlight progress and a platform to drive further improvements in patient care.
At FH Europe Foundation, we strongly support the principles behind European Patients’ Rights Day. Our work – focused on improving awareness, diagnosis and treatment of inherited lipid conditions such as familial hypercholesterolaemia (FH), Homozygous FH (HoFH), elevated Lp(a) and Familial Chylomicronaemia Syndrome (FCS) – is rooted in the belief that all patients deserve timely, accurate and person-centred care.
Outlined in the European Charter of Patients’ Rights, these rights form the backbone of a healthcare system that respects human dignity and promotes equity:
European Patients’ Rights Day is a timely reminder of the essential role that rights-based care plays in creating resilient, patient-focused healthcare systems. At FH Europe Foundation, we remain committed to working with our partners across Europe and beyond, to ensure that the voices of patients – especially those living with inherited lipid conditions – are heard, valued and protected.
By championing these rights together, we can help shape a future where all individuals receive the care, respect and support they deserve.
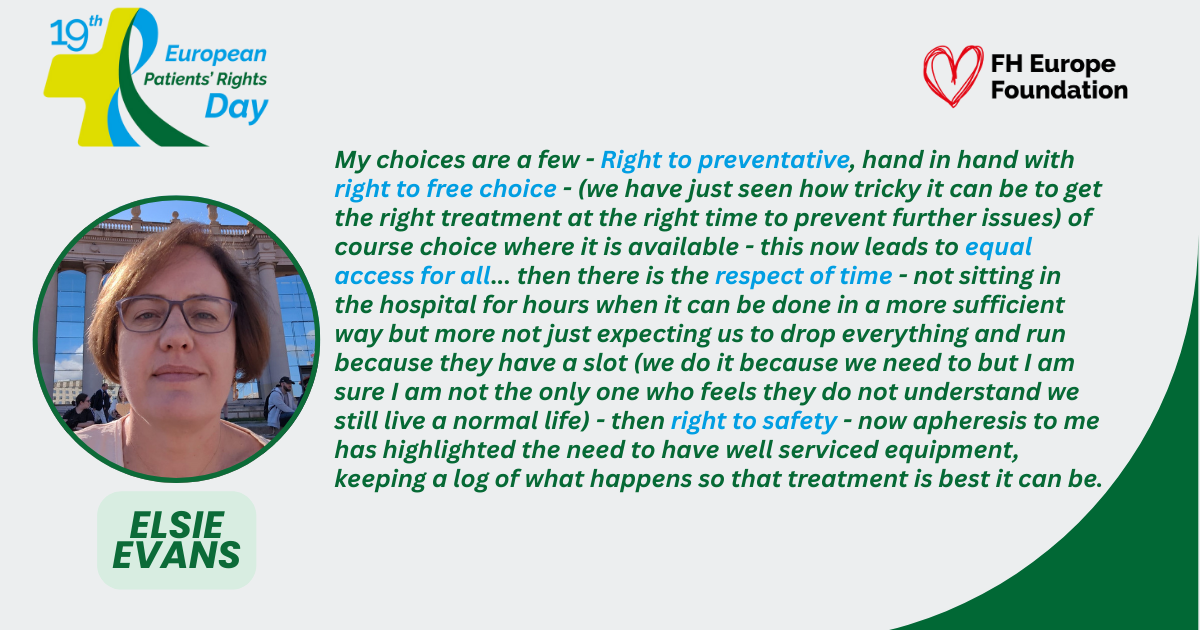
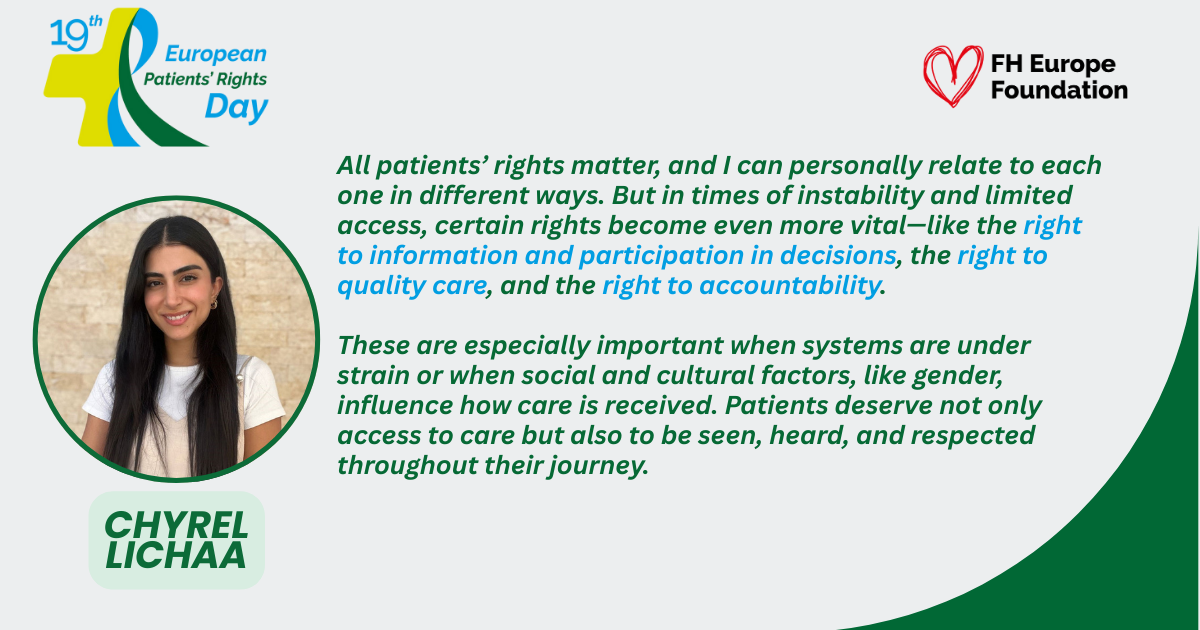
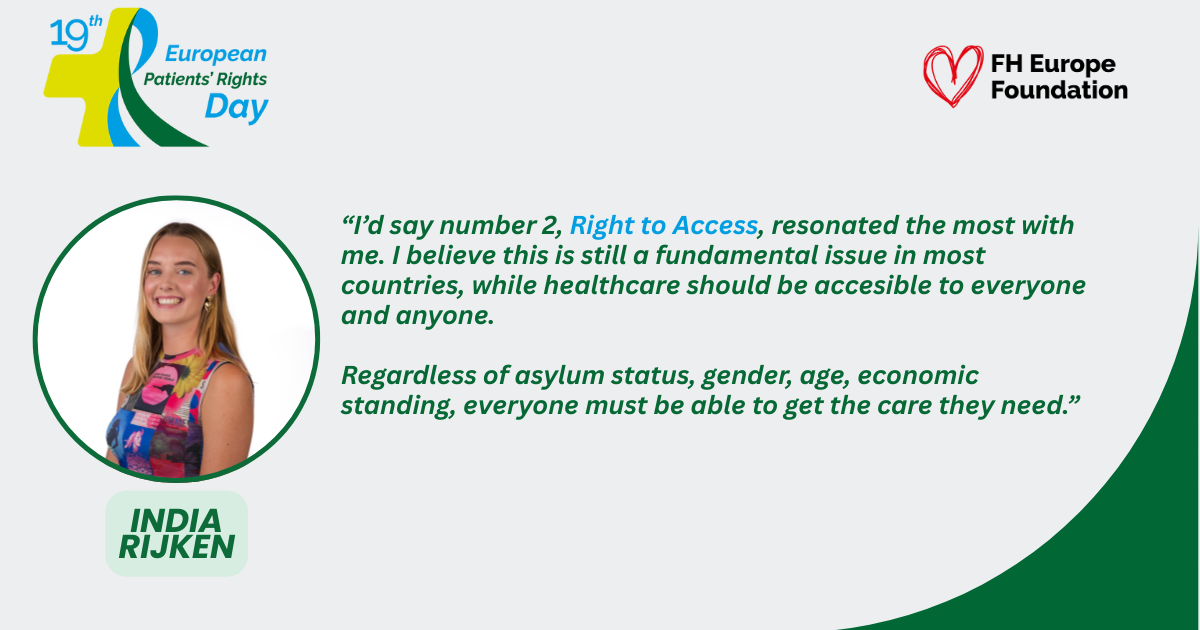
As part of our contribution to this year’s European Patients’ Rights Day, we are also sharing personal reflections from our community – sharing some of there views on what these rights mean in their daily lives. Alongside each of the 14 rights, you’ll find links to stories, insights and testimonials from individuals living with FH and related conditions, highlighting how these rights play out in practice and where gaps still remain.
These real-life experiences offer valuable context to the Charter and strengthen the call for health systems that truly put people first.



Explore the highlights from FH Europe's April 2025 Heart Beat newsletter to catch up on the latest updates in cardiovascular health, policy, and patient advocacy:
Subscribe to the Heart Beat News.
Explore the highlights from FH Europe's March 2025 Heart Beat newsletter to catch up on the latest news and events in the world of cardiovascular health:
Subscribe to the Heart Beat News.
Amsterdam, March 31, 2025 – More than 1.4 billion people worldwide are living with elevated Lipoprotein(a) [Lp(a)], an inherited cardiovascular risk factor that often goes undetected. Despite its clear link to heart attacks, strokes, peripheral arterial disease and aortic stenosis, only 1%-2% of the population is tested, leaving millions vulnerable to preventable cardiovascular events.
The economic burden of cardiovascular diseases (CVD) is staggering, with the EU alone spending €282 billion annually on healthcare and productivity losses related to CVD. This highlights the urgent need for improved prevention and early detection strategies, especially for high-risk conditions like elevated Lp(a).
To address this, the first-ever Global Summit on Elevated Lp(a), 24-25 March, Brussels, brought together over 60 global scientific and medical leaders, policymakers, advocates and and patient representatives. Hosted under the patronage of the Polish EU Presidency, the Summit coincided with Lp(a) Awareness Day (24th March) and aimed to ensure Lp(a) testing becomes routine, and that everyone is tested free of charge, at least once and as early as possible in their lifetime.
The Summit was led by the Lp(a) International Task Force and organised by the FH Europe Foundation under the scientific leadership of Professor Florian Kronenberg (Austria). Discussions focused on systemic barriers to Lp(a) testing, the lived experiences and challenges of those living with elevated Lp(a) levels, who issued a clear call to action: “Test, test, test”, as well as the emerging opportunities to drive policy and clinical change.
The Summit aligned with current EU health policy developments, including the ambitions of a dedicated Cardiovascular Health Plan, European Health Data Space (EHDS) launch and the December 2024 Council Conclusions on Cardiovascular Health, to integrate Lp(a) testing into national CVD risk assessments and enhance preventive care.
Cost savings, not only cost effectiveness
Prof. Zanfina Ademi from Monasch University in Australia, presented the results of the first International Cost-Effectiveness Study on Lp(a) Testing, which demonstrated unequivocally the economic viability of widespread Lp(a) testing commissioned by the Lp(a) International Task Force, under the FH Europe Foundation.
The Brussels International Declaration on Lp(a) - A Call to Action
The Summit informed the Brussels International Declaration on Lp(a), which outlines concrete steps for governments and health systems to implement routine testing for elevated levels of Lp(a), with endorsements expected from leading global and national health organizations. The declaration recognises the public health impact of testing for elevated Lp(a), as an important independent risk factor for CVD, and its effective management, would be enormous, and should be a key pillar of countries’ prevention strategies worldwide. The key five asks of the declaration to national, regional and international policymakers are:
Transformational digital tools and ethical artificial intelligence were recognised as key enablers for the implementation of systematic Lp(a) testing and the effective, personalised management of elevated Lp(a) levels. In line with the commitments set out in the Brussels Declaration, progress would be driven through cross-border shared learning, robust impact assessment, and comprehensive monitoring and evaluation on an annual basis.

MEP Romana JERKOVIĆ, Chair of the MEP Cardiovascualr Health Group and Host of the Summit said “As Chair of the MEP Group on Cardiovascular Health, I am thrilled to have co-hosted this important international summit, which is the first time there has been a dedicated meeting bringing together people with lived experiences, scientists, practitioners, and policymakers together to align on the concrete actions needed to make systematic testing of elevated Lp(a) and effective management for all who need it for all a reality. I am really excited to see this meeting of minds and ideas”. She added “I will be taking the Brussels International Declaration on Lp(a) to the MEP Cardiovascular Health Group and ask for their endorsement. The train has left the station and it is imperative we act in this space”.
Among political leaders, MEP Adam JARUBAS , Chair of the Health Committee in the European Parliament, SANT, underlined “I am fully supportive of a European Plan on Cardiovascular Health to address the huge financial and human burden of Europe’s biggest killer. Such a plan will accelerate much needed progress in policy, programmes, investment and research, also at national level. And your technical meeting demonstrated clearly why Lp(a), inherited lipid conditions must feature prominently in such a plan. We need to be bold and ambitious in this space.” He further stressed the importance of equity “As a transversal topic, a core priority for the SANT committee is health inequalities both among and within EU countries and beyond – health may depend largely on a DNA code – as we are discussing today – but should never depend on a postal code”.
Prof. Florian Kronenberg, Chair of the Lp(a) International Task Force highlighted: “It is not only that the scientific evidence is overwhelming. Enormous monetary savings are possible by introducing a more systematic measurement of Lp(a) in combination with the other traditional risk factors followed by the appropriate preventive treatment. Thereby much of the associated impairment of our fellow citizens through frequent heart attacks and strokes could be prevented. A shift from “we try to fix the damage” - which is often not possible - into the direction “prevent the preventable” has to be the focus of the upcoming years. Each year of prevention we lose for the given individual, puts her/him at more danger."
“The Lp(a) Global Summit was more than a scientific gathering - it was a powerful reminder that we live and act within a complex system, where no single factor exists in isolation. Lp(a) is not just a biomarker - it is a crucial signal in a web of genetic, environmental, social and behavioural interactions that shape cardiovascular health. Recognizing and addressing Lp(a) means embracing complexity, breaking silos, and designing truly personalized prevention strategies. The Summit illuminated a path forward: one that demands systems thinking, transdisciplinary collaboration, and bold action to bridge the gap between knowledge and real world impact” said Dr Marius Geanta, President Center for Innovation in Medicine and Member of the Lp(a) International Taskforce.
Magdalena Daccord, CEO of FH Europe Foundation concluded "The first-ever Lp(a) Global Summit was a landmark moment, bringing together leading experts, policymakers, industry as well as advocates and people living with elevated Lp(a) to address one of the greatest gaps in cardiovascular prevention. Its strength lay in unprecedented collaboration—where lived experience met scientific excellence, and political will aligned with urgent public health needs. Now, this momentum must translate into lasting, cross-border action to ensure equitable access to Lp(a) testing and care. The future of cardiovascular health depends on it."
The Lp(a) Global Summit was organised with the support of experts, volunteers, and in partnership with World Heart Federation, International Atherosclerosis Society, European Alliance for Cardiovascular Health, European Society of Atherosclerosis and Global Heart Hub, industry partners such as Amgen, Novartis, Roche Diagnostics, and Silence Therapeutics. It marks a pivotal shift toward proactive cardiovascular health, aiming to prevent, not just treat, heart disease.
A dedicated webinar to reflect on the first Lp(a) Global Summit, elevated Lp(a) as a CVD risk factor and the science behind it, economic implications of testing for Lp(a) and ambitions for the Brussels International Declaration will take place later today, 31 March 2025 between18:00 and19:00 CET.
Please click here to register.
For more information, contact:
Magdalena Daccord
CEO, FH Europe Foundation
Email: lpaglobalsummit@fheurope.org