Yesterday, February 20th, our very own Patient Ambassador and Community Engagement Manager, Emma Print represented the patients’ perspective on a multidisciplinary panel at a virtual event hosted by the European Federation of Pharmaceutical Industries and Associations (EFPIA).
The virtual event highlighted the importance of having national cardiovascular plans that included secondary prevention measures. It featured insights from different stakeholders in the context of a recently published report by the London School of Economics (LSE), offering an invaluable opportunity to understand the practical applications of this research. The panellists included a patient, (Emma Print), a researcher (Panos Kanavos, Associate Professor of International Health Policy at the LSE), a politician (Tomislav Sokol, Member of the European Parliament, EPP Group, Croatia), and an industry representative (Haseeb Ahmad, President of Novartis Europe).

Cardiovascular disease remains the number 1 killer in Europe, costing the EU 282 billion euros per year. In addition to mortality, morbidity and cost, the experience of a heart attack or stroke can also have a profound and lasting impact on the quality of life of those affected, as well as their families or carers.
The report, commissioned by the EFPIA Cardiovascular Health Platform, demonstrates that if 70% of people living with cardiovascular disease could have their risk factors better managed, 1.2 million deaths in the EU could be averted over the next ten years. For example, reducing LDL-cholesterol levels by just 1 mmol/L has been shown to reduce all-cause mortality by 10%.
You can access the report here.
For the recording of the event please visit: https://efpia.eu/news-events/events/efpia-event/getting-to-the-heart-of-the-matter-improving-cardiovascular-health-in-europe/
We are pleased to welcome Gráinne Crowley to our team as FHEF Partnerships and Development Lead, starting today, February 1st, 2024. Gráinne brings over 15 years of experience in patient advocacy and health policy, working within the biotech industry. Before joining the pharma industry, Gráinne was an EU policy advisor for a leading independent research charity and worked as a Principal Consultant for a Public Affairs company advising companies, trade associations and NGOs on EU policy and engagement. She is a former co-chair of EuropaBio’s Patient Engagement Forum and participated in IMI projects with a specific focus on enhancing patient involvement in R&D. In her spare time, she enjoys rediscovering her home country (Ireland), water sports and is an avid rugby fan.
In her role as Partnerships and Development Lead, Gráinne will be responsible for developing and fostering meaningful relationships with the wider health industry, including life sciences, MedTech, diagnostics as well as the emerging players in the health innovation space, which share a common mission with FHEF, to further our Foundation’s aims and objectives. Moving on, Gráinne will lead the Industry Roundtable, while ensuring all our activities are in line with the governing compliance and ethics rules as well as agreements in place between FHEF and our Industry Partners.
This is an important step for our growing organisation. It demonstrates FH Europe Foundation’s commitment to building robust, compliant, and transparent collaboration with the life sciences players. We are entering an important phase with our foundation, with projects and initiatives which have the potential to shape the future of the patients and their families we represent as well as the wider familial dyslipidaemias community.
A warm welcome to the Team and the FH Europe community, Gráinne!
'We look forward to building on Gráinne’s rich experience and knowledge, to help improve our ongoing interactions with the existing industry partners by ensuring they are built on strong and transparent foundations, while we expand our partnerships and collaborations with new partners. Those are exciting times at FHEF, and we need to ensure, that whatever we do, we bring the best outcomes to our network, patients, their relatives and families, and the citizens, within the right framework.' – said Magdalena Daccord, Chief Executive of FH Europe Foundation.
'I am really thrilled to be part of the FH Europe Foundation and to work with its dynamic and passionate team. I know I will learn a tremendous amount from my new colleagues while, at the same time, have the opportunity of staying in touch with former ones. I look forward to continuing to support meaningful partnerships between the patient community, industry and other stakeholders but from a new and exciting perspective' said Gráinne.
If you would like to connect with Gráinne to join FH Europe Foundation roundtable of industry partners, to explore opportunities to be part of the Lp(a) International Taskforce or any other collaboration and initiatives, please contact her via email gc@fhef.org.
31 January 2024, Amsterdam, The Netherlands
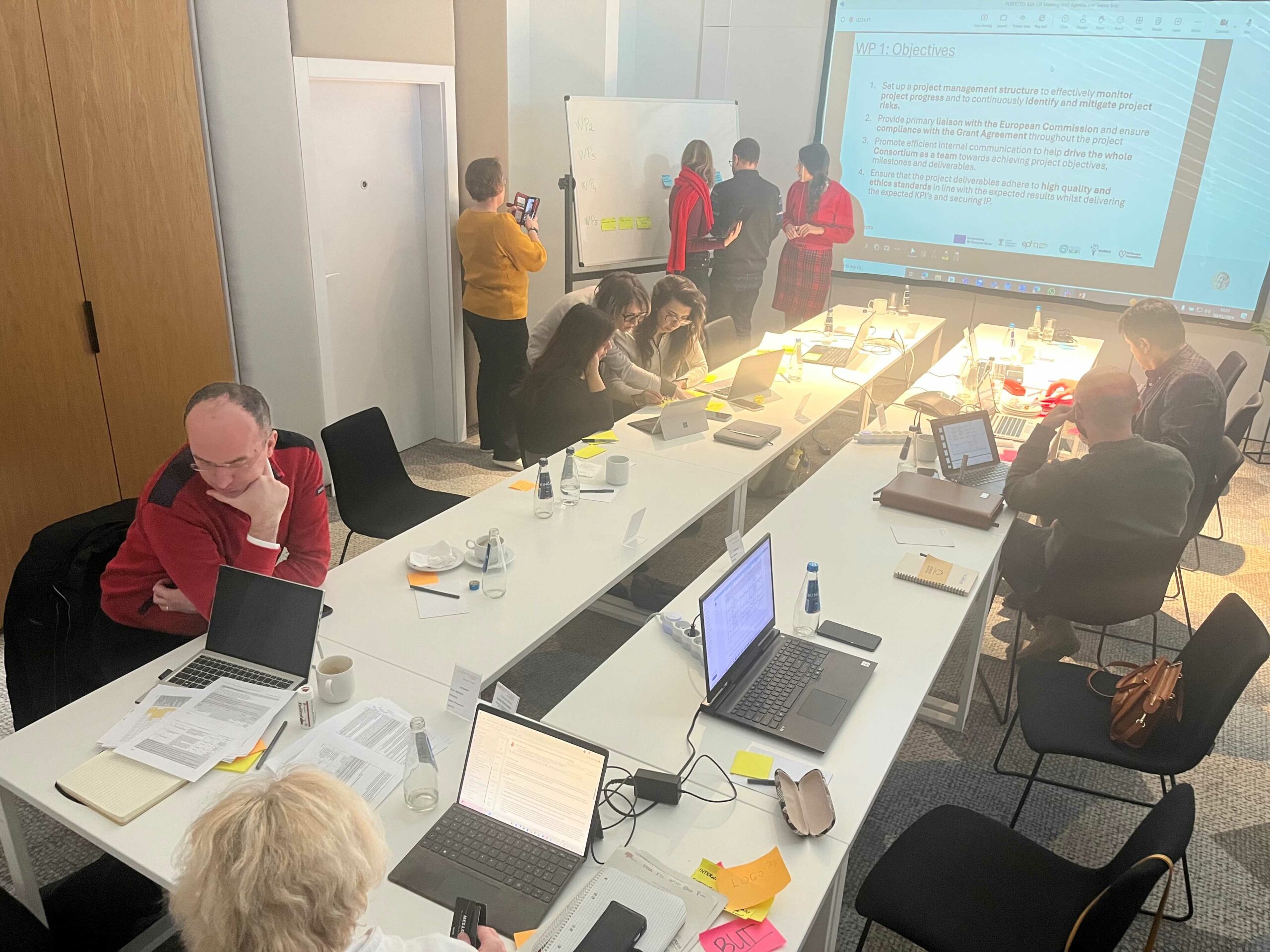
We are delighted to announce that the PERFECTO project, co-funded by the European Union, has officially been launched, with a kick-off meeting of consortium partners in Warsaw on 29 and 30 January. The project was successfully selected in response to an EU4Health call for proposals on prevention of NCDs - cardiovascular diseases, diabetes and other NCDs from September 2022.
PERFECTO stands for “Preventing thE PReventable – Familial HypErCholesterolaemia paediaTric screening for cardiOvascular health”. It is a landmark initiative for personalized prevention, tackling an often overlooked genetic/hereditary cause of cardiovascular disease through the lens of social innovation. And its mission is to generate evidence for the implementation of FH Paediatric Screening across Europe – which will have significant positive impact for individuals affected, their relatives, and the wider society, as well as healthcare systems, which are often at breaking point post-pandemic.
The project concept was developed by a consortium of diverse partners and experts from the fields of patient advocacy, screening implementation, HTA, health equity and citizens’ and social sciences.
The Consortium’s composition, Work Packages (WP) and Leaders
The PERFECTO consortium consists of 6 partners responsible for 5 WPs and is led by FH Europe Foundation, as the Coordinator.
The two-days long launch meeting, moderated by FH Europe Foundation’s Sr Policy Advisor – Nicola Bedlington, was attended by all the Partners and expert advisors, as well as representatives of the European Commission with Yvette Azzopardi from DG Sante and Hulya Okuyan, the Project Officer from HaDEA.
“Together with FH patients, advocates and ambassadors, clinicians, scientists, policymakers and health systems experts, we embark on this journey to bring innovative solutions to the forefront of CVD prevention. This multidisciplinary collaboration underscores our commitment to empowering communities and ensuring a healthier future for generations to come.” – said Magdalena Daccord.

Familial Hypercholesterolaemia (FH) is the world’s most common monogenic disorder, affecting 1 in 300 people. This means 2.5 million Europeans, with 2 million adults and 500,000 children have FH. Yet, to date only est. 10% are diagnosed and treated causing a huge burden of CVD, which is preventable. FH is marked by high levels of low-density lipoprotein (LDL), commonly known as the ‘bad’ cholesterol, from a young age. This compound accumulates in the arteries from birth and poses a very high risk of developing increasing atherosclerotic cardiovascular disease (ASCVD) risk at an early age. In fact, compared to the general population between the ages of 20 and 40, these individuals are twenty times more likely to develop significant cardiac complications, such as angina or myocardial infarction (commonly known as a heart attack).
Early screening, detection and personalised prevention which means appropriate treatment combined with healthy lifestyle habits, is key to a “normal and a CVD-free” life.

At the core of PERFECTO is to move forward the implementation of FH Paediatric Screening across Europe by creating a more enabling and supporting environment, focussing especially on countries where CVD burden is the highest and FH awareness is lower among wider stakeholders. PERFECTO, based on the FH Europe Network experiences and current activities of awareness, recognizes that there is an unmet need and gap in the understanding of the attitudes and decision-making processes of stakeholders necessary to moving forward with implementation of FH Paediatric Screening. PERFECTO will use a bottom-up, citizen-led approach to develop and fine-tune a personalised communication model that could be generalised beyond FH and could be used/replicated for other condition with risk factors that are common for the majority of NCDs such as cancer and metabolic disorders. PERFECTO will build on advocacy efforts at the European level on the topic of FH Paediatric Screening but also aim to reach the entire population, not only diagnosed patients, as this is an essentially undiagnosed disease, to empower parents to seek and accept information and relevant screening. Special focus will be on populations that are typically not included in health policy design, in this case the Roma population in Romania, and their perceptions, barriers and knowledge base addressed in the proposed Personalised Communications Model (PCM). The project aims to transcend barriers (physical, cognitive, cultural, language) with the use of open and innovative practices in a digital era through the development of an integrated digital PCM to improve the scope and content (knowledge/literacy, skills/competences, self-efficacy/empowerment) and provide an alternative model/complementary learning environment orientated towards real needs and concerns to enable the uptake of FH Paediatric Screening with a framework adaptable to other EU countries to improve both health literacy and policy advocacy potentially for all countries within the consortium’s coverage (EU-wide and beyond). By doing so, PERFECTO will have a true patient and citizen driven approach with a strong capacity building element for multiplication, specifically in countries among population groups in need. It will address the knowledge gaps referred to earlier, adding relevant evidence to the state-of-the-art, with substantial impact envisaged in FH Paediatric Screening implementation, and ultimately contributing to the reduction of CVD burden and health inequity.
The project comes to life at an important time, when the European CVD community actively advocates for a joint response to the CVD as the public health burden. FH Europe Foundation is a Partner of the European Alliance for Cardiovascular Health (EACH), advocating for a European Cardiovascular Health Plan. PERFECTO is being launched 3 weeks following the launch of PerMed FH, a precision medicine project for FH. With the launch of the Joint Action on Cardiovascular Diseases and Diabetes later in 2024, also co-funded by the EU4Health Programme, PERFECTO will seek to identify and to amplify any synergies in the mission to eliminate the burden of CVD and diabetes in Europe through screening and early detection, considering social and personal barriers and opportunities.
More information on the project, the work packages and the progress will be communicated through a dedicated webpage, which will be announced in the upcoming weeks. Please follow #PERFECTO, #FHchildscreeening, #FindFH and #EU4Health #HealthUnion #CVD #CVH #NCD #personalisedprevention for additional information. And register to our newsletter to receive regular updates, if you have not done so yet.
Stichting FH Europe Foundation (FH Europe) (NL): The Foundation’s main focus is advocacy and patient support, it drives public health policy improvements and collaborates progressively with leading European and the EU institutions – like the European Commission, the European Parliament and many other EU stakeholders. FH Europe Foundation is the next stage in the evolution of FH Europe (fheurope.org), the European Network of FH patient organisations. FH Europe and its Network has a leading place in the European public health policy space responding to the unmet needs of patients and people affected with inherited lipid conditions. FH Europe Foundation’ member patient organisation in Bulgaria will play an active role in testing/ validating materials and outputs from WP3. FH Europe is aware that the Bulgarian health system has implemented cholesterol screening at age 16. Building on this, Bulgaria aspires to implement a fully-fledged FH Paediatric Screening Programme, which could leverage the results and learnings from PERFECTO.
EuroScan (DE): The network acquired legal status in 2017, becoming EuroScan International Network e. V., a not-for-profit scientific association registered in Germany connecting public agencies, scientific organisations and individuals across all continents. EuroScan has been and aims to remain the main global forum for sharing and developing of methods for early identification and pre-assessment of emerging, new, and obsolete health technologies. EuroScan membership comprises several organisations around the world including members in four continents but mainly based in Europe (NIHR UK, Agenas IT, Osteba SP, AETSA SP, NIPHNO NO, Inca FR) and Asia Pacific (MaHTAs Ma, NECA SK, Singapore HTA, CDN TW; Australia and New Zealand). EuroScan holds a MoU with several organisations including WHO, HTAi; INAHTA, HTAsiaLink and REDETSA. EuroScan has been collaborating in several EU funded projects among those it can be mentioned the active Horizon 2020 SAFENMEDTECH (https://safenmt.com/ ) and the IMI EU-PEARL (https://eu-pearl.eu/).
Cyprus University of Technology (CUT) (CY): CUT is the second largest and one of the leading research Universities in Cyprus, that has high values regarding its academic character and its emphasis on high quality research in major branches of science and technology. It has a staff of approximately 300 academics, approximately 400 Researchers and Special Scientists, and 219 administrative employees supporting all aspects of teaching and research. Research emphasis at CUT is reflected in the substantial funding provided to academics for the establishment of research centres and laboratories, the support it provides for collaborations with world renowned Universities and Institutions, and the participation of its faculty in several national and European research projects. The University is pioneering in the production of applied research and achieving excellence in the international research area. In order to meet the challenges of society and industry, the results of the research produced at the University are transferred as know-how to society, industry and productive organisations to create innovative solutions with significant economic, social and environmental benefits. In the context of research, innovation and entrepreneurship activities, new jobs and opportunities are created for young scientists in cutting-edge sectors.
Centre for Innovation in Medicine (InoMed) (RO): InoMed is a non-governmental organisation based in Bucharest, with a focus on innovation in healthcare. It aims to shorten the time between the emergence of innovations in the medical sector and their application for patients' benefit in Romania and elsewhere. The Center develops programs to educate, inform and engage all audiences about innovation in medicine to create a friendly environment for early adoption of innovative technologies, ideas, products and services. InoMed also serves as an independent platform for informed dialogue between stakeholders in the field of omics medicine, personalised (precision) medicine, digital health, data oncology, immune-oncology, cancer research, biotechnology, systems biology and other hot scientific topics. InoMed is active in dedicated communication, education, advocacy and policy channels but also research activities.
European Public Health Alliance (EPHA) (BE): A member-led organisation made up of public health NGOs, patient groups, health professionals and disease groups, we work to improve health and strengthen the voice of public health in Europe. EPHA has a solid network of 80 members dedicated to providing better health for all across the EU, through umbrella organisations and national members. Together with them, EPHA advocates for public health solutions leading to better health for all based on its values of equity, solidarity, sustainability, universality, diversity and good governance. Through its Roma Health Network, EPHA is also one of the leading NGO alliances for the voice in Roma health.
Embrace the excitement of the upcoming year with FH Europe Foundation's Events Calendar for 2024! As we gear up for a thrilling year ahead, our dedicated team has prepared this calendar with easy colour-coded highlights, making it your go-to guide for the exciting events on our radar:
From key awareness days and events marked in red, signifying major initiatives and campaigns where your involvement is crucial, to relevant awareness days and events in dark blue, encouraging your engagement through likes, shares, and comments for a broader impact. Additionally, discover days worth knowing about in the context of health and well-being, marked in light blue.
Open and download the 2024 Awareness Days and Events Calendar.
Be part of the action and let´s make 2024 a year of shared moments, impactful campaigns, and a healthier world. Join us on this exciting journey!