A silent connection between the mind and the heart
Every beat of the heart is influenced not only by biology, but by our thoughts, emotions, and sense of safety. Mental health, as how we think, feel, and cope, is inseparable from cardiovascular health. Yet for many living with inherited lipid disorders or other lifelong cardiovascular conditions, mental well-being remains the missing piece of care.
Living with a genetic lipid disorder, such as familial hypercholesterolaemia (FH), often begins with a diagnosis that reshapes a person’s self-image and future. The lifelong treatment journey, regular monitoring, lifestyle adjustments, and awareness of family risk can lead to chronic stress, anxiety, or depression. These feelings are not weakness, they are valid and biologically meaningful responses that, when unaddressed, can influence cardiovascular outcomes themselves.
The latest European Society of Cardiology (ESC) Clinical Consensus Statement on Mental Health and Cardiovascular Disease (2025) makes this connection unequivocally clear: mental health and cardiovascular disease (CVD) interact bidirectionally, each influencing the onset, course, and prognosis of the other.
The WHO’s 2025 call to action: Integrating mind and body
In June 2025, the World Health Assembly adopted Resolution WHA78, a landmark decision advancing the global agenda for noncommunicable diseases (NCDs) and mental health. The resolution explicitly links the NCD and mental health agendas, urging countries to integrate mental health promotion, prevention, and care into chronic disease services, and to address shared risk factors such as stress, stigma, and social inequality.
This recognition is critical. Cardiovascular diseases remain the leading cause of death globally and people with mental health conditions are at significantly higher risk of developing CVD, experiencing worse outcomes, and dying earlier than those without mental health challenges. Conversely, people diagnosed with CVD face a high prevalence of depression (up to 18%) and anxiety, according to the ESC statement.
The WHO resolution reinforces that mental health is not optional in chronic disease care, it is a determinant of survival and quality of life.
From evidence to empathy: What the science tells us
The 2025 ESC Consensus Statement synthesises decades of research and expert consensus, revealing several key insights:
For individuals living with inherited lipid disorders, these findings carry special relevance. Many experience “invisible stressors”: genetic guilt, fear of transmitting risk to children, or uncertainty about future cardiac events. These chronic emotional burdens can elevate stress hormones, impair sleep, and erode motivation to sustain lifestyle and medication adherence.
Bridging two worlds: The ESC’s “Psycho-Cardio” approach
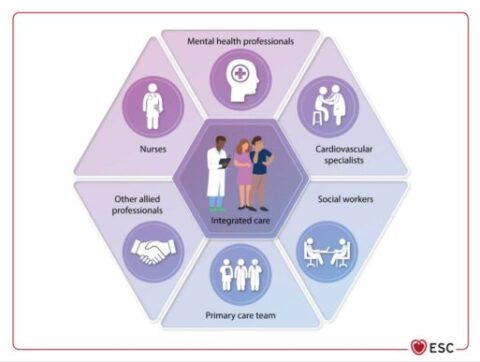
One of the most transformative recommendations from the ESC is the creation of multidisciplinary “Psycho-Cardio Teams” care models that unite cardiologists, mental health professionals, nurses, and allied specialists in shared decision-making.
This model promotes the ACTIVE principles for care:
Such an integrated approach moves beyond treating cholesterol levels or blood pressure — it treats the whole person.
Inherited lipid disorders: Why mental health must be part of care
People with inherited lipid disorders often receive early and repeated exposure to medical surveillance. This can create “disease fatigue,” feelings of guilt or frustration about family implications, and a sense of isolation when peers don’t share the same health concerns.
Addressing mental health in this group is not only compassionate but clinically relevant:
Screening for mental health conditions should therefore become standard practice in lipid and cardiology clinics. Validated tools such as the Patient Health Questionnaire (PHQ) or Hospital Anxiety and Depression Scale (HADS) can be implemented easily and lead to early support or referral.
Caring for caregivers, too
The ESC statement also highlights the often-overlooked mental health of informal caregivers: parents managing their child’s lipid disorder, partners supporting someone after a cardiac event, or families dealing with generational risk. Emotional burnout among caregivers can diminish the entire family’s well-being and adherence to care plans. Recognising and supporting caregivers is an essential component of heart-healthy care.
"One day my daughter got diagnosed with Familia Chylomicronaemia Syndrome, FCS. Living with FCS means struggling everyday. It doesn't just affect her; it affects our whole family. I have lost my job, my health, both mental and physical. Rare diseases need your attention, your support, don't forget this."
Teevi Pobus,
a mother whose daughter is living with FCS
Turning awareness into action
For clinicians, policymakers, and patient communities, the path forward is clear:
As the WHO resolution underscores, integrating mental health into NCD services is both a human rights issue and a health systems priority.
A message for our community
To everyone living with an inherited lipid disorder or cardiovascular disease: your mental health matters as much as your lipid numbers. Feelings of fear, frustration, or sadness are not signs of failure, they are signals that your heart and mind need care together. Seeking psychological support is an act of strength, not weakness.
This World Mental Health Day, let’s take a collective step towards holistic heart care where emotional well-being and cardiovascular health beat in harmony.
Prepared by
 Dr. Marina Leroy,
Dr. Marina Leroy,
FH Europe Foundation Scientific Communications Manager
References